How Place and Health Interact
Places where people reside hold the key to the state of health and disease manifest within and on bodies. However, connecting downstream health problems (e.g., chronic diseases) to upstream issues and characteristics of communities is challenging for most medical models and tools (1, 2).
The presence of “ downstream” health problems ( i.e., obesity, diabetes, heart disease) for large groups of people suggest that causation and solutions to health problems go beyond individual bodies defined as patients to incorporate a set of systemic institutional, social, and structural issues for bodies now defined as social beings (1, 3). Two principles of importance in place-health research are the social construction of places and embodiment.
Human geography contributes the social construction of place. Bodies that have been imprinted with external physical and social worlds are also firstly groups engaged in the social construction of places where they embellish a space with remembrances, imaginings, social relations, and the public assimilation of shared narratives (4-6).
The theory of embodiment explains how the external physical and social worlds are taken in and expressed in human biology (7-13).
Figure 1 demonstrates how both the social construction of places by groups and embodiment work together to configure and distribute opportunities in relation to socioeconomic status, race, and ethnicity (13-23).
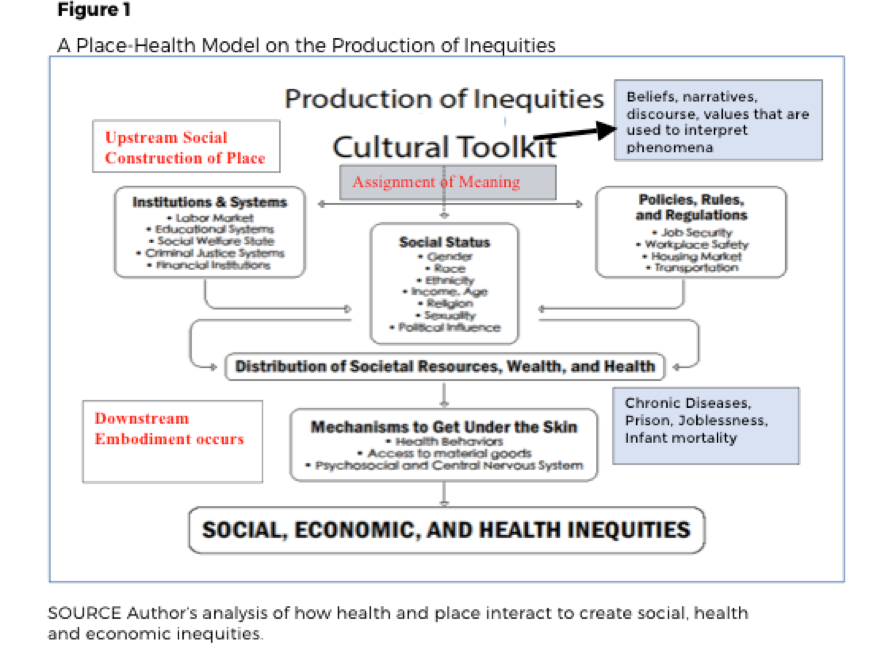
According to the place-health model in Figure 1, differences in health, social, and economic status at the bottom of the model originate at the top with the cultural toolkit that is attached to a place or region(24). The toolkit is where the construction of place begins as social processes assign meaning to phenomena using a shared set of norms, system of beliefs, narratives, and distinctive spiritual, material, intellectual, and emotional features (25-28). It is through the public assimilation of shared narratives in any given society that groups begin to convert spaces into places (29-31).
In Figure 1 once the cultural toolkit ascribes meaning and a shared narrative, groups use those ideas to assign worth to the social status of others and sanction the distribution of societal opportunities and resources also referred to as the social determinants of health (SDOH). Further, below the cultural toolkit, other influential arenas result from the assigned meanings including (a) the institutions, policies, and systems that govern a place, and (3) the policies, rules and regulations of that place. These mutually reinforcing arenas are the SDOH in a given region that serve to regulate the place in which the citizens live(32, 33).
Finally, the bottom of the model demonstrates the concept of embodiment when it portrays how the SDOH, (i.e., experiences, opportunities, and resources) of a place get under the skin of marginalized groups by three routes: (1) influencing behavior and making behavior harmful; (2) restricting the distribution of and access to key resources; and/or ( 3) by causing deep seated, chronic anxiety and physiological stress (18, 24, 34-37).
A final principle of the place-health model are the Upstream and Downstream designations to the left of the diagram noting that a society can intentionally use its collective autonomy to work in any or all of these areas: 1) downstream, where illness already exist; 2) upstream on the structural issues including policies, systems, or regulations); or 3) furthest upstream on the cultural toolkit to explore and change the socially constructed, values, beliefs, and narratives that drive the assignment of meaning to group differences and other phenomena (2).
1. Hansen H, Metzl J. Structural Competency in the U.S. Healthcare Crisis: Putting Social and Policy Interventions Into Clinical Practice. Journal of Bioethical Inquiry. 2016;13(2):179-83.
2. Andress L. Using a social ecological model to explore upstream and downstream solutions to
rural food access for the elderly. Cogent Medicine. 2017;4(1):1393849.
3. Hansen H, Braslow J, Rohrbaugh RM. From Cultural to Structural Competency-Training
Psychiatry Residents to Act on Social Determinants of Health and Institutional Racism. JAMA psychiatry. 2018;75(2):117-8.
4. Low SM. Towards an anthropological theory of space and place. Semiotica. 2009;2009(175):21-37.
5. Low SM. Embodied space (s) anthropological theories of body, space, and culture. Space and
Culture. 2003;6(1):9-18.
6. Low SM. Spatializing culture: the social production and social construction of public space in
Costa Rica. American ethnologist. 1996;23(4):861-79.
7. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health
inequities in the USA: evidence and interventions. The Lancet.389(10077):1453-63.
8. Krieger N. Proximal, Distal, and the Politics of Causation: What’s Level Got to Do With It?
American Journal of Public Health. 2008;98(2):221-30.
9. Krieger N. Public health, embodied history, and social justice: Looking forward. International
Journal of Health Services. 2015;45(4):587-600.
10. Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective.
International journal of epidemiology. 2001;30(4):668-77.
11. Krieger N. Embodiment: a conceptual glossary for epidemiology. Journal of Epidemiology & Community Health. 2005;59(5):350-5.
12. Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Social science & medicine. 1994;39(7):887-903.
13. Petteway R, Mujahid M, Allen A. Understanding Embodiment in Place-Health Research:
Approaches, Limitations, and Opportunities. Journal of Urban Health. 2019:1-11.
14. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic
Americans in the 21st century. Proceedings of the National Academy of Sciences. 2015;112(49):15078-83.
15. Marmot M. Creating healthier societies. Bulletin of the World Health Organization.
2004;82(5):320-.
16. Marmot MG, Bell R. Action on health disparities in the United States: commission on social determinants of health. Jama. 2009;301(11):1169-71.
17. Singh-Manoux A, Marmot M. Role of socialization in explaining social inequalities in health. Social science & medicine. 2005;60(9):2129-33.
18. Adler NE, Stewart J. Preface to the biology of disadvantage: socioeconomic status and health.
Annals of the New York Academy of Sciences. 2010;1186(1):1-4.
19. Auchincloss AH, Gebreab SY, Mair C, Diez Roux AV. A review of spatial methods in epidemiology, 2000–2010. Annual review of public health. 2012;33:107-22.
20. Blanchard AK, Prost A, Houweling TAJ. Effects of community health worker interventions on
socioeconomic inequities in maternal and newborn health in low-income and middle-income countries:
a mixed-methods systematic review. BMJ Glob Health. 2019;4(3):e001308.
21. Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health
outcomes: a critical review. Journal of Epidemiology & Community Health. 2001;55(2):111-22.
22. Roux AVD. Neighborhoods and health: Oxford University Press; 2018.
23. Swinnerton S. Living in poverty and its effects on health. Contemporary Nurse. 2006;22(1):75-80.
24. Andress L. The emergence of the social determinants of health on the policy agenda in Britain: A case study, 1980–2003: The University of Texas School of Public Health; 2006.
25. Dorfman L, Wallack L, Woodruff K. More than a message: framing public health advocacy to change corporate practices. Health education & behavior. 2005;32(3):320-36.
26. Wallack L, Lawrence R. Talking about public health: Developing America’s “second language”.
American Journal of Public Health. 2005;95(4):567-70.
27. Goffman E. Frame analysis: An essay on the organization of experience1974. null p.
28. Jameson F. On Goffman's Frame Analysis. Theory and Society. 1976;3(1):119-33.
29. Kim J-H. Understanding Narrative Inquiry: The Crafting and Analysis of Stories as Research: SAGE Publications; 2015.
30. Saltmarshe E. Using Story to Change Systems. Stanford Social Innovation Review; 2018.
31. Tsui E, Starecheski A. Uses of oral history and digital storytelling in public health research and practice. Public health. 2018;154:24-30.
32. Friel S, Marmot MG. Action on the social determinants of health and health inequities goes global. Annu Rev Public Health. 2011;32.
33. Marmot M. Social determinants of health inequalities. Lancet. 2005;365.
34. Adler N, Rehkopf D. US disparities in health: descriptions, causes, and mechanisms. Annual review of public health. 2008;29:235.
35. McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33-44.
36. Wallace D, Wallace R. Life and death in Upper Manhattan and the Bronx: toward an evolutionary perspective on catastrophic social change. Environment and Planning A. 2000;32(7):1245-66.
37. Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308(5722) 648-52.